October 22, 2014
Epidural Analgesia: To Delay or Not to Delay, That Is the Question
By: Henci Goer, BA | 0 Comments
By Henci Goer
Unless you have been 'off the grid' on a solitary trek, surely you have read and heard the recent flurry of discussion surrounding the just released study making the claim that the timing of when a woman receives an epidural ('early' or 'late' in labor) made no difference in the rate of cesarean delivery. Your students and clients may have been asking questions and wondering if the information is accurate. Award winning author and occasional Science & Sensibility contributor Henci Goer reviews the 9 studies that made up the Cochrane systematic review: Early versus late initiation of epidural analgesia for labour to determine what they actually said. Read her review here and share if you agree with all the spin in the media about this new research review. Additionally, head on over to the professional and parent Lamaze International sites to check out the new infographic on epidurals to share with your students and clients.- Sharon Muza, Science & Sensibility Manager.
 Articles have been popping up all over the internet in recent weeks citing a new Cochrane systematic review- Early versus late initiation of epidural analgesia for labour, concluding that epidural analgesia for labor needn't be delayed because early initiation doesn't increase the likelihood of cesarean delivery, or, for that matter, instrumental vaginal delivery (Sng 2014). The New York Times ran this piece. Some older studies have found that early initiation appeared to increase likelihood of cesarean (Lieberman 1996; Nageotte 1997; Thorp 1991), which is plausible on theoretical grounds. Labor progress might be more vulnerable to disruption in latent than active phase. Persistent occiput posterior might be more frequent if the woman isn't moving around, and fetal malposition greatly increases the likelihood of cesarean and instrumental delivery. Which is right? Let's dig into the review.
Articles have been popping up all over the internet in recent weeks citing a new Cochrane systematic review- Early versus late initiation of epidural analgesia for labour, concluding that epidural analgesia for labor needn't be delayed because early initiation doesn't increase the likelihood of cesarean delivery, or, for that matter, instrumental vaginal delivery (Sng 2014). The New York Times ran this piece. Some older studies have found that early initiation appeared to increase likelihood of cesarean (Lieberman 1996; Nageotte 1997; Thorp 1991), which is plausible on theoretical grounds. Labor progress might be more vulnerable to disruption in latent than active phase. Persistent occiput posterior might be more frequent if the woman isn't moving around, and fetal malposition greatly increases the likelihood of cesarean and instrumental delivery. Which is right? Let's dig into the review.
The review includes 9 randomized controlled trials of 'early' versus 'late' initiation of epidural analgesia. Participants in all trials were limited to healthy first-time mothers at term with one head-down baby. Five trials further limited participants to women who began labor spontaneously, three mixed women being induced with women beginning labor spontaneously, and in one, all women were induced. Analgesia protocols varied, but all epidural regimens were of modern, low-dose epidurals. So far, so good.
Examining the individual trials, though, we see a major problem. You would think that the reviewers would have rejected trials that failed to divide participants into distinct groups, one having epidural initiation in early labor and the other in more advanced labor, since the point of the review is to determine whether early or late initiation makes a difference. You would think wrong. Of the nine included trials, six failed to do this.
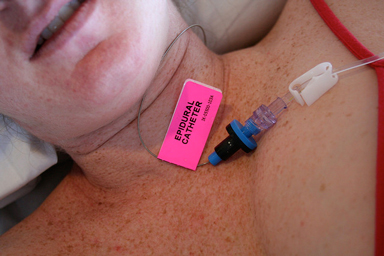
cc photo bryanrmason http://flickr.com/photos/b-may/397189835
The two Chestnut trials (1994a; 1994b) had the same design, differing only in that one was of women who were laboring spontaneously at trial entry and the other included women receiving oxytocin for induction or augmentation. Women were admitted to the trial if they were dilated between 3 and 5 cm. Women in the early group got their epidural immediately while women in the late group could have an epidural only if they were dilated to 5 cm or more. If late-group women were not dilated to 5 cm, they were given systemic opioids and could have a second dose of opioid one hour later. They could have an epidural when they attained 5 cm dilation or regardless of dilation, an hour after the second opioid dose. Let's see how that worked out.
Among the 149 women in the trial that included women receiving oxytocin (Chestnut 1994b), median dilation in the early group at time of epidural initiation was 3.5 cm, meaning that half the women were dilated more and half less than this amount. The interquartile deviation was 0.5 cm, which means that values were fairly tightly clustered around the median. The authors state, however, that cervical dilation was assessed using 0.5 increments which meant that dilation of 3-4 cm was recorded as 3.5. In other words, women in the early group might have been dilated to as much as 4 cm. The median dilation in the late group was 5.0 cm, again with a 0.5 cm interquartile deviation. Some women in the late group, therefore, were not yet dilated to 5 cm when their epidural began, and, in fact, the authors report that 26 of the 75 women (35%) in the late group were given their epidural after the second dose of opioid but before attaining 5 cm dilation. The small interquartile deviation in the late group tells us that few, if any, women would have been dilated much more than 5 cm. Add in that assessing dilation isn't exact, so women might have been a bit more or less dilated than they were thought to be, and it becomes clear that the 'early' and 'late' groups must have overlapped considerably. Furthermore, pretty much all of them were dilated between 3 and 5 cm when they got their epidurals, which means that few of these first-time mothers would have been in active labor, as defined by the new ACOG standards.
Overlap between early and late groups must have been even greater in Chestnut et al.'s (1994a) trial of 334 women laboring spontaneously at trial entry because median dilation in the early group was greater than in the other trial (4 cm, rather than 3.5) while median dilation in the late group was the same (5.0 cm), and interquartile deviation was even tighter in the late group (0.25 cm, rather than 0.5 cm). As before, dilation was measured in 0.5 cm increments, which presumably means that women in the early group dilated to 4-5 cm would have been recorded as '4.5,' thereby qualifying them for the 'early' group even though they might have been as much as 5 cm dilated.
Based on my analysis, I would argue that there was no clinically meaningful difference in dilation between early and late groups in either trial.
A second pair of trials, one a mixed trial of spontaneous labor onset and induction and the other all induced, also had the same design in both trials (Wong 2005; Wong 2009). All women were less than 4 cm dilated at first request for pain medication. In the early group, women had an opioid injected intrathecally, i.e. the 'spinal' part of a combined spinal-epidural, and an epidural catheter was set. At the second request, an epidural was initiated. In the late group, women were given a systemic opioid. At second request, they were given a second dose of systemic opioid if they hadn't reached 4 cm dilation and an epidural if they had dilated to 4 cm or more. At third request, they were given an epidural regardless of dilation. Women who had no vaginal exam at second request and were given an epidural were 'assumed,' in the authors' words, to be dilated to at least 4 cm. What were the results?
Wong (2005) included 728 women, some beginning labor spontaneously and some induced. You may already have noticed the flaw in the trials' design: Wong and colleagues confused the issue by considering intrathecal opioid to be equivalent to epidural anesthetic in the early group, although women didn't actually receive anesthetic until their second request for pain medication some unknown time later. So far as I know we have no evidence that opiods, spinal or epidural, have any effect on labor progress. As to dilation at the time of epidural initiation, 63% of women in the so-called 'early' group were either determined or assumed to be at 4 cm dilation or more while in the late group, some unknown proportion were less than 4 cm dilated either because they got their epidural at third pain medication request regardless of dilation or they were assumed to be at 4 or more cm dilation at second request, but weren't assessed.
Wong (2009), a study of 806 induced women, was set up the same way but reported data somewhat differently. Early-group women were administered a spinal opioid at a median of 2 cm dilation and an interquartile range of 1.5 to 3 cm, which means that values in the middle 50% of the dataset ranged from 1.5 to 3 cm. We have no information on dilation at the time they received their epidural. The median dilation at which late-group women had their epidural initiated was 4 cm with an interquartile range of 3 to 4 cm, that is, in the middle 50% of the dataset ranged from 3 to 4 cm dilation.
As with the Chestnut trials, dilation at time of epidural initiation in the two Wong trials must have overlapped considerably between groups. And, again, few women in the late epidural group would have been in active labor. The Wong trials, however, muddy the waters even further by considering spinal opioid to be the same thing as epidural anesthetic, and while the authors were careful to use the term 'neuraxial analgesia,' the Cochrane reviewers made no such distinction.
This brings us to Parameswara (2012), a trial of 120 women that included both spontaneous onset and induced labors. This trial defined the early group as women less than 2 cm dilated at time of epidural initiation and the late group as women more than 2 cm dilated. That's all the information they provide on group allocation.
Last of the six, we have Wang (2011), a trial of 60 women in spontaneous labor. All women were given intrathecal anesthetic plus opioid. The early group was started on epidural anesthetic plus opioid 20 minutes later whereas the late group had their epidural initiated when they requested additional pain relief. No information is given on dilation at time of epidural initiation. Not only do we have no idea whether early and late groups differed from one another, women in both groups received neuraxial anesthetic at the same time.
In summary, 'garbage in, garbage out.' No conclusions can be drawn about the effect of early versus late epidural administration from these six studies.
The other three studies are a different story. They achieve a reasonable separation between groups. Luxman (1998) studied 60 women with spontaneous labor onset. The early group had a mean, i.e., average, dilation of 2.3 cm with a standard deviation of + or - 0.6 cm while the late group had a mean dilation of 4.5 cm + or - 0.2 cm. Ohel (2006) studied a mixed spontaneous onset and induced group of 449 women. The mean dilation at initiation in the early group was 2.4 cm with a standard deviation of 0.7 cm, and the late group had a mean dilation of 4.6 cm with a standard deviation of 1.1 cm. Wang (2009), the behemoth of the trials, included 12,629 women who began labor spontaneously. The early epidural group had a median dilation of 1.6 cm with an interquartile range of 1.1 to 2.8 and the late group a median of 5.1 cm dilation with an interquartile range of 4.2 to 5.7. Cesarean and instrumental delivery rates were similar between early and late groups in all three trials, so had reviewers included only these three trials, they would still have arrived at the same conclusion: early epidural initiation doesn't increase likelihood of cesarean and instrumental delivery.
We're not done, though. Wang (2009) points us to a second, even bigger issue.
The Wang (2009) trial, as did all of the trials, limited participants to healthy first-time mothers with no factors that would predispose them to need a cesarean. The Wang trial further excluded women who didn't begin labor spontaneously. Nevertheless, the cesarean rate in these ultra-low-risk women was an astonishing 23%. Comparing the trials side-by-side reveals wildly varying cesarean and instrumental vaginal delivery rates in what are essentially homogeneous populations.
Comparing the trials uncovers that epidural timing doesn't matter because any effect will be swamped by the much stronger effect of practice variation.
Analysis of the trials teaches us two lessons: First, systematic reviews can't always be taken at face value because results depend on the beliefs and biases that the reviewers bring to the table. In this case, they blinded reviewers from seeing that two-thirds of the trials they included weren't measuring two groups of women, one in early- and one in active-phase labor. Second, practice variation can be an unacknowledged and potent confounding factor for any outcome that depends on care provider judgment.
Conclusion
So what's our take home? Women need to know that with a judicious care provider who strives for spontaneous vaginal birth whenever possible, early epidural administration won't increase odds of cesarean or instrumental delivery. With an injudicious one, late initiation won't decrease them. That being said, there are other reasons to delay an epidural. Maternal fever is associated with epidural duration. Running a fever in a slowly progressing labor could tip the balance toward cesarean delivery as well as have consequences for the baby such as keeping the baby in the nursery for observation, testing for infection, or administering prophylactic IV antibiotics. Then too, a woman just might find she can do very well without one. Epidurals can have adverse effects, some of them serious. Comfort measures, cognitive strategies, and all around good emotionally and physically supportive care don't. Hospitals, therefore, should make available and encourage use of a wide range of non-pharmacologic alternatives and refrain from routine practices that increase discomfort and hinder women from making use of them. Only then can women truly make a free choice about whether and when to have an epidural.
After reading Henci's review and the study, what information do you feel is important for women to be aware of regarding epidural use in labor? What will you say when asked about the study and timing of an epidural? You may want to reference a previous Science & Sensibility article by Andrea Lythgoe, LCCE, on the use of the peanut ball to promote labor progress when a woman has an epidural. ' SM
References
Caughey, A. B., Cahill, A. G., Guise, J. M., & Rouse, D. J. (2014). Safe prevention of the primary cesarean delivery. American journal of obstetrics and gynecology, 210(3), 179-193.
Chestnut, D. H., McGrath, J. M., Vincent, R. D., Jr., Penning, D. H., Choi, W. W., Bates, J. N., & McFarlane, C. (1994a). Does early administration of epidural analgesia affect obstetric outcome in nulliparous women who are in spontaneous labor? Anesthesiology, 80(6), 1201-1208.http://www.ncbi.nlm.nih.gov/pubmed/8010466?dopt=Citation
Chestnut, D. H., Vincent, R. D., Jr., McGrath, J. M., Choi, W. W., & Bates, J. N. (1994b). Does early administration of epidural analgesia affect obstetric outcome in nulliparous women who are receiving intravenous oxytocin? Anesthesiology, 80(6), 1193-1200.http://www.ncbi.nlm.nih.gov/pubmed/8010465?dopt=Citation
Lieberman, E., Lang, J. M., Cohen, A., D'Agostino, R., Jr., Datta, S., & Frigoletto, F. D., Jr. (1996). Association of epidural analgesia with cesarean delivery in nulliparas. Obstet Gynecol, 88(6), 993-1000. http://www.ncbi.nlm.nih.gov/pubmed/8942841
Luxman, D., Wolman, I., Groutz, A., Cohen, J. R., Lottan, M., Pauzner, D., & David, M. P. (1998). The effect of early epidural block administration on the progression and outcome of labor. Int J Obstet Anesth, 7(3), 161-164. http://www.ncbi.nlm.nih.gov/pubmed/15321209?dopt=Citation
Nageotte, M. P., Larson, D., Rumney, P. J., Sidhu, M., & Hollenbach, K. (1997). Epidural analgesia compared with combined spinal-epidural analgesia during labor in nulliparous women. N Engl J Med, 337(24), 1715-1719. http://www.ncbi.nlm.nih.gov/pubmed/9392696?dopt=Citation
Ohel, G., Gonen, R., Vaida, S., Barak, S., & Gaitini, L. (2006). Early versus late initiation of epidural analgesia in labor: does it increase the risk of cesarean section? A randomized trial. Am J Obstet Gynecol, 194(3), 600-605. http://www.ncbi.nlm.nih.gov/pubmed/16522386?dopt=Citation
Parameswara, G., Kshama, K., Murthy, H. K., Jalaja, K., Venkat, S. (2012). Early epidural labour analgesia: Does it increase the chances of operative delivery? British Journal of Anaesthesia 108(Suppl 2):ii213 - ii214. Note:This is an abstract only so all data from it come from the Cochrane review.
Sng, B. L., Leong, W. L., Zeng, Y., Siddiqui, F. J., Assam, P. N., Lim, Y., . . . Sia, A. T. (2014). Early versus late initiation of epidural analgesia for labour. Cochrane Database Syst Rev, 10, CD007238. doi: 10.1002/14651858.CD007238.pub2 http://www.ncbi.nlm.nih.gov/pubmed/25300169
Thorp, J. A., Eckert, L. O., Ang, M. S., Johnston, D. A., Peaceman, A. M., & Parisi, V. M. (1991). Epidural analgesia and cesarean section for dystocia: risk factors in nulliparas. Am J Perinatol, 8(6), 402-410. http://www.ncbi.nlm.nih.gov/pubmed/1814306?dopt=Citation
Wang, F., Shen, X., Guo, X., Peng, Y., & Gu, X. (2009). Epidural analgesia in the latent phase of labor and the risk of cesarean delivery: a five-year randomized controlled trial. Anesthesiology, 111(4), 871-880. http://www.ncbi.nlm.nih.gov/pubmed/19741492?dopt=Citation
Wang, L. Z., Chang, X. Y., Hu, X. X., Tang, B. L., & Xia, F. (2011). The effect on maternal temperature of delaying initiation of the epidural component of combined spinal-epidural analgesia for labor: a pilot study. Int J Obstet Anesth, 20(4), 312-317.http://www.ncbi.nlm.nih.gov/pubmed/21840705
Wong, C. A., McCarthy, R. J., Sullivan, J. T., Scavone, B. M., Gerber, S. E., & Yaghmour, E. A. (2009). Early compared with late neuraxial analgesia in nulliparous labor induction: a randomized controlled trial. Obstet Gynecol, 113(5), 1066-1074.http://www.ncbi.nlm.nih.gov/pubmed/19384122?dopt=Citation
Wong, C. A., Scavone, B. M., Peaceman, A. M., McCarthy, R. J., Sullivan, J. T., Diaz, N. T., . . . Grouper, S. (2005). The risk of cesarean delivery with neuraxial analgesia given early versus late in labor. N Engl J Med, 352(7), 655-665. http://www.ncbi.nlm.nih.gov/pubmed/15716559?dopt=Citation
About Henci Goer
Henci Goer, award-winning medical writer and internationally known speaker, is the author of The Thinking Woman's Guide to a Better Birth and Optimal Care in Childbirth: The Case for a Physiologic Approach, She is the winner of the American College of Nurse-Midwives 'Best Book of the Year' award. An independent scholar, she is an acknowledged expert on evidence-based maternity care.
Tags
Labor Childbirth education Cesarean Epidural Professional Resources Labor/Birth Systematic Review Maternal Infant Care Henci Goer Pain Medication