August 26, 2013
Perception of Social Support and Increased Risk of PPD in Cities: Research Review
By: Walker Karraa, PhD | 0 Comments
Today, regular Science & Sensibility contributor Walker Karraa shares a study that came out earlier this summer examining the incidence of postpartum depression and place of residence (rural vs urban.) Women living in urban areas were more likely to suffer from PPD. Are you surprised? Why do you think that might be? Take a look at the information Walker shares and join the conversation in the comments section. If you work in an urban setting, are you doing everything you can to help mothers with this increased risk? Let us know. - Sharon Muza, Community Manager
A new Canadian study has examined the relationship between place of residence and risk of developing postpartum depression (PPD) based on population-based sample. Vigod, Tarasoff, Bryja, Dennis, Yudin, & Ross (2013) presented Relation between place of residence and postpartum depression in the early release at Canadian Medical Association. The study is a comprehensive and complex analysis of the statistical indicators related between where women live and the risk for developing postpartum depression (PPD.) For childbirth professionals who practice in urban settings, the findings here underscore the need for heightened awareness of the issues of support and awareness regarding maternal mental health in pregnancy and postpartum.
An overview of the study objectives, design, methods, and results has been compiled. Finally, a brief discussion as to the role of childbirth professionals is offered, and resources are provided.
Objectives
The objectives of this study were as follows:
- To compare the risk of PPD among Canadian women living in rural and urban areas
- To identify factors that could explain any associations between place of residence and risk of postpartum depression (Vigod, et al., 2013, p. 1)
Design
Sample: Women who had recently given birth and responded to the 2006 Canadian Maternity Experiences Survey through the Public Health Agency of Canada and the Canadian Perinatal Surveillance System were contacted. The study is a comprehensive and complex analysis of the statistical indicators related between where women live and the risk for developing PPD.
Stratified sampling by province or territory ensured sample size and a simple random sample without replacement was pulled from each stratum. Inclusion consisted of women age over 15 who had singleton birth and were living with their child at the time of the interview. Response rate of 78% were collected via telephone and computer assisted interview resulting in 6421 of 8244 women contacted, representing 76, 500 Canadian women nationally. The final sample was 6126.
Outcome Measure: All women were administered the Edinburgh Postnatal Depression Scale (EPDS; Cox, Holden, Sagovsky, 1987). Risk of PPD was operationalized as anyone with a score of < 13 points.
Definitions of populations. The authors defined the types of populations as follows:
- Rural: populations outside the settlements of 1000 or more people or outside areas with a population density of 400 more inhabitants per square kilometer (p. 2)
- Semi-rural: population <30,000
- Semi-urban: population 30,000-499,999
- Urban: > 500,000
Additionally, the authors implemented a metropolitan-influence component in defining and compartmentalizing different populations:
To separate the women with the most potential for social isolation from those with less potential for isolation, we further divided women living in rural and small town areas by 'metropolitan-influenced zone'. These zones indicate the percentage of residents who commute to urban centers. The zones are designated as strong (> 30% residents commute to urban core), moderate (5%-29% commute), weak (> 0%, but <5%) or no (0%) metropolitan influence. (Vigod, et al., 2013, p. 2)
Methods
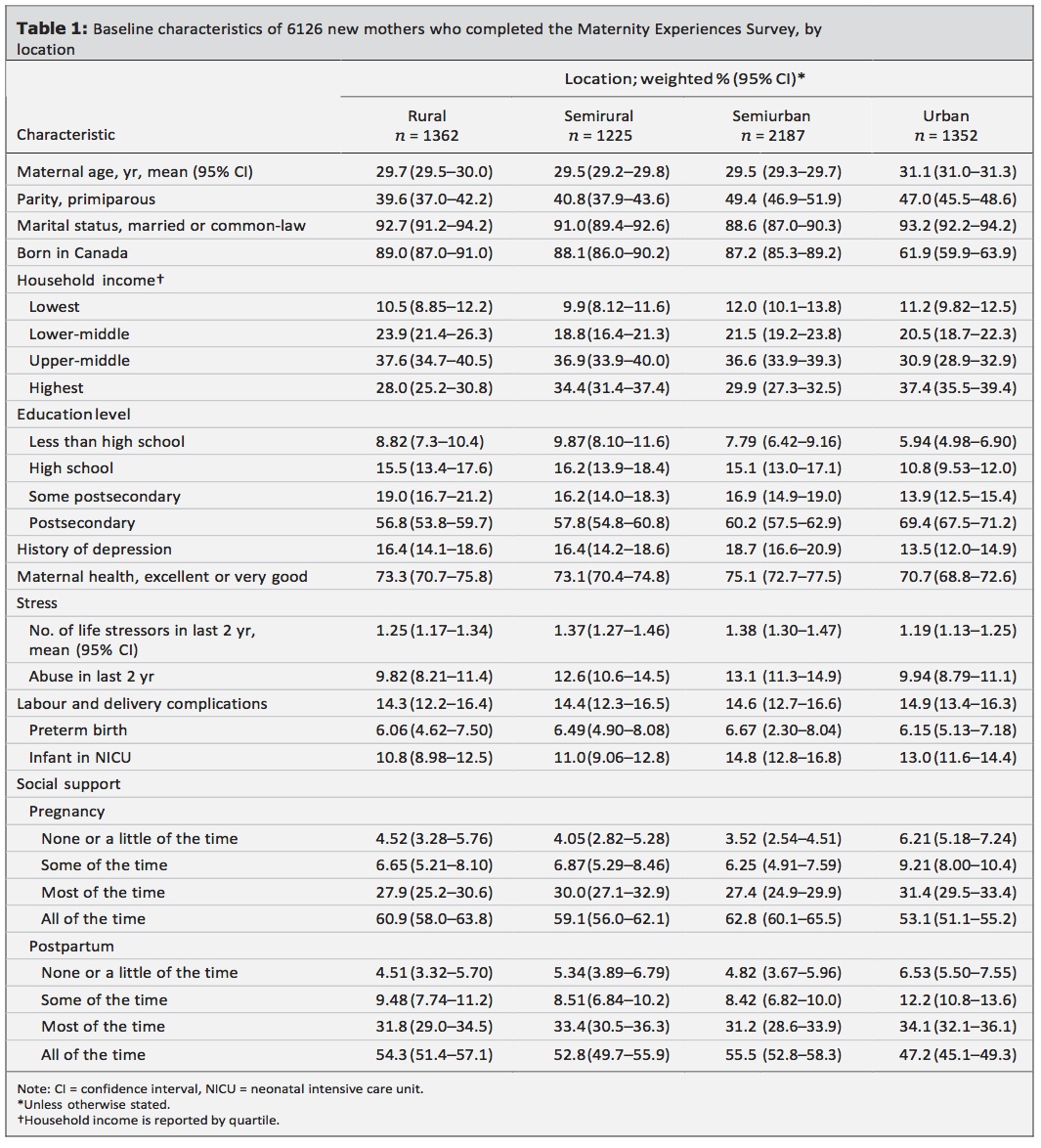
A thorough panel of covariates was administered to data analysis, including: age, parity, marital status, SES, educational status, and country of birth, recent immigration (within 5 years), and distance travelled to birth. In addition, history of depression, substance/alcohol use and life stressors such as interpersonal violence, abuse, and social support during pregnancy and postpartum period were factored. Medical covariates of complications during perinatal period included preterm birth, birth weight, NICU, and cesarean section. All data were analyzed through SAS version 9.3.
Findings
We found that Canadian women who lived in large urban areas (i.e., population > 500,000 inhabitants) were at higher risk of postpartum depression than women living in other areas. The risk factors for postpartum depression (including history of depression, social support and immigration status) that were unequally distributed across geographic regions accounted for most of the variance in the rates of postpartum depression. (Vigod et al., 2013, p. 5)
The authors noted that immigration status, interpersonal violence, and self-perceived health and social support were responsible for the variance. For example, in the area of perceived social support in pregnancy and postpartum, the following findings were noted in the table below.
Conclusions
The authors noted that modifiable risk factors included social support in pregnancy and postpartum. Childbirth professionals working in cities can provide invaluable social connectivity and access to key resources targeting this issue. Issues of dislocation, immigration status, and domestic violence are risk factors for higher incidence of PPD that need to be addressed in education, training and curriculum. Resources for domestic violence and legal advocacy have been provided. Each professional can create ways to offer the material to students and clients that remains within a scope of practice as defined by their certifying organization, and that resonates with his/her personal style and community needs. Please feel free to add to the list of resources!
Resources
Postpartum Support International (resources in Spanish as well)
Interpersonal violence resources
National Domestic Violence Hotline: Staffed 24 hours a day by trained counselors who can provide crisis assistance and information about shelters, legal advocacy, health care centers, and counseling.
1-800-799-SAFE (7233); 1-800-787-3224 (TDD)
Domestic Violence Fact Sheets
Domestic Violence State Hotlines
Learn more for your own continuing education at the Department of Justice Office of Violence Against Women.
References
Cox, J. L., Holden, J. M., & Sagovsky, R. (1987). Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. The British journal of psychiatry, 150(6), 782-786.
Vigod, S. N., Tarasoff, L. A., Bryja, B., Dennis, C. L., Yudin, M. H., & Ross, L.E. (2013). Relation between place of residence and postpartum depression. Journal of Canadian Medical Association. doi:10.1503/cmaj.122028.
Tags
Postpartum depression Postpartum Research Walker Karraa PPMAD Guest Posts Postpartum Mood Disorders PPD