August 21, 2012
One in Three Suffers Posttraumatic Stress Disorder: A Look Behind the Headlines
By: Sharon Muza, BS, LCCE, FACCE, CD/BDT(DONA), CLE | 0 Comments
by David White, MD CCFP, Associate Professor, Dept of Family & Community Medicine, University of Toronto
Dr. David White reviews the study "Postpartum Post-Traumatic Stress Disorder Symptoms: The Uninvited Birth Companion" that made news headlines earlier this month. This post, is part two of a two part series. (Read part one here, where Penny Simkin discussed how the media created sensationalistic headlines from the study.) Dr. White demonstrates how important it is to go to the source, and evaluate the study design for oneself. I appreciate Dr. White sharing his summary and review of the research behind the study. - SM

Creative Commons Image by Horia Varlan
The dramatic headline caught my eye: "One in Three Post-Partum Women Suffers PTSD Symptoms After Giving Birth: Natural Births a Major Cause of Post-Traumatic Stress, Study Suggests."[i] As a family doctor who provides maternity care, I was both puzzled and alarmed. Where were all these women? Each year, I care for about 50 women through pregnancy, birth and post-partum. Am I failing to recognize the 16 or 17 who develop PTSD? Are they suffering without proper care?
The article claimed "Of the women who experienced partial or full post-trauma symptoms, 80 percent had gone through a natural childbirth, without any form of pain relief."
On reflection, I became skeptical. So I read the original research paper.[ii] To their credit, the authors acknowledge, "Controversy remains whether childbirth should be included under the definition of a traumatic event that meets the criteria for post-traumatic stress disorder." Unfortunately, their own study is so riddled with problems that it can only add confusion.
First, there is the matter of selection: 102 women agreed to participate, 89 completed the two assessments. There is no mention of how many women were approached, or how many women had births at the hospital during the study period. So there is no way to assess possible selection bias. Suspicion is warranted when a crucial methodological detail is omitted.
Then there is the issue of diagnostic criteria. The diagnosis of PTSD requires that the symptoms last more than one month and cause significant impairment in social, occupational, or other important areas of functioning (both DSM-IV-TR and ICD-10). The researchers administered their survey instrument within a few days of birth and again at one month post-partum. The latter just barely meets the criterion for duration. And could there be a cuing effect from administering an initial questionnaire within a few days of birth?
The findings report "full PTSD", "partial PTSD" and "PTSD symptomatology". However the tool used by the researchers, a self-administered questionnaire called Posttraumatic Stress Diagnostic Scale (PDS®), indicates only whether someone meets the DSM diagnostic criteria or not.[iii]
Now to the analysis, which piles questionable analysis onto this shaky diagnostic platform. "For processing the data we needed to select a group large enough to be statistically significant but homogenous enough to offer meaningful results." So they lump together those missing one or two symptoms with those who actually have PTSD. The justification for this methodological legerdemain is that others have done it. They reference a study by Stein, Walker et al[iv] that is considerably more careful. It differs substantially in that it used telephone interviews, a different assessment tool and analyzed full and partial PTSD separately.
The results are reported in a way that even makes it difficult to determine what group they are analyzing. Is it the "full PTSD" (3) + "Partial PTSD" (7) = 10? No, it is 3 ("full) + 4 ("missing 1 or 2 symptoms") =7. But look at Table 2, showing 5 in the row labeled "PTSD". Table 3 has it back up to 7.
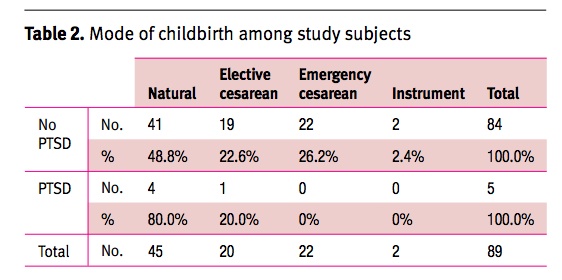
Table source: http://www.ima.org.il/imaj/ar12jun-02.pdf
The terminology for the groups seems variable. At times it is "PTSD group", at others it is "women with PTSD symptoms" and the Tables simply apply the label "PTSD."
Terminology problems continue: "control group" is used regularly to denote those who did not manifest PTSD symptoms, an odd usage for a study in which there is no intervention or randomization.
While studying Table 2, check out the mode of delivery: Natural 45, Cesarean 42 (20 elective), Instrumental 2. That indicates a Cesarean section rate of 47%. Could this be a biased sample?
More fun with numbers: the text reports that 80% of women with PTSD symptoms reported feeling very uncomfortable in the undressed state: Table 3 shows 3 out of 7 reporting this.
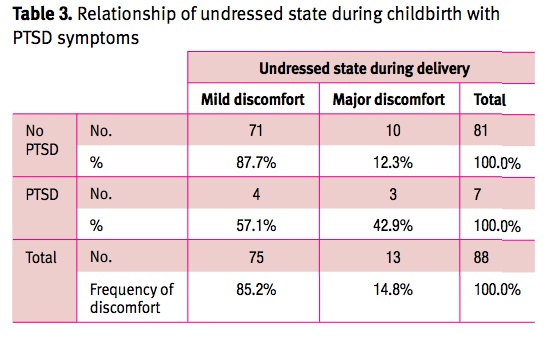
Table source: http://www.ima.org.il/imaj/ar12jun-02.pdf
And the figure that 80% of those with PTSD had gone through natural labour? It appears to come from Table 2, showing that 4 out of 5 women in the "PTSD" group had "Natural" childbirth. I scoured the tables and text in vain to find why the PTSD group is 5 in Table 2 and 7 in Table 3.
The definitions of mode of delivery should be more precise. The authors describe natural births as "non-interventional" but we really don't know about analgesia use in this group. This matters, because they found "A significantly smaller number of women who developed PTSD symptoms received analgesia during delivery compared to the control group." For this to make sense, it is essential distinguish vaginal births with and without effective pain relief.
This definitional and analytic fog leads to the conclusion that a lot of women have PTSD symptoms following birth. The authors don't trouble themselves to explain why their numbers don't square with the excellent community-prevalence study in the references, in which "The estimated prevalence of full PTSD was 2.7% for women and 1.2% for men. The prevalence of partial PTSD was 3.4% for women and 0.3% for men."4
This study brings discredit to an admittedly difficult field, one in which researchers must address the criticism of medicalizing normal life experiences.
I'm a GP, not an expert in PTSD. But I think I can recognize "significant impairment in social, occupational, or other important areas of functioning." The important issue for practitioners is whether we identify and help those at risk and who need assistance. Screening for post-partum depression is important. Adding a simple open-ended question such as "tell me about your birth" is likely to yield much more benefit in practice than this study.
I appreciate Dr. White's analysis and wonder how many other professionals bothered to examine the research behind the headlines, in order to come to their own conclusions about the study design, assumptions and findings. What do you think of this research? Did you understand the terms being used or how the results were determined? Do you think any journalists who wrote the sensational headlines took the time to look at the study themselves? It is always important to be a critical thinker for yourself, examine the information and ask questions. Sometimes, the research does not match up with the front page news, or the study may not have been well-designed. Please share your thoughts, questions and comments here, with Dr. White, Penny Simkin, myself and Science & Sensibility readers. - SM
References
[i] American Friends of Tel Aviv University (2012, August 8). One in three post-partum women suffers PTSD symptoms after giving birth: Natural births a major cause of post-traumatic stress, study suggests. ScienceDaily. Retrieved August 14, 2012, from http://www.sciencedaily.com /releases/2012/08/120808121949.htm
A useful review of the PDS® is at: http://occmed.oxfordjournals.org/content/58/5/379.full.pdf+html
[iv] Stein, M. B., Walker, J. R., Hazen, A. L., & Forde, D. R. (1997). Full and partial posttraumatic stress disorder: Findings from a community survey. The American Journal of Psychiatry, 154(8), 1114-9. Retrieved from http://search.proquest.com/docview/220491145?accountid=14771
A useful overview of PTSD at
http://www.ptsd.va.gov/professional/pages/ptsd-overview.asp
A review of research issues in PTSD following childbirth:
Pauline Slade: Towards a conceptual framework for understanding post-traumatic stress symptoms following childbirth and implications for further research. Journal of Psychosomatic Obstetrics & Gynecology (January 2006), 27 (2), pg. 99-105, accessed at http://resolver.scholarsportal.info.myaccess.library.utoronto.ca/resolve/0167482x/v27i0002/99_tacffucaiffr
About David White
 David White is a community-based family doctor in Toronto and Associate Professor of Family & Community Medicine at the University of Toronto. (DFCM, U of T). He currently serves as the Interim Director of UTOPIAN, the practice-based research network comprising all teaching sites affiliated with the Department of Family & Community Medicine at the University of Toronto.
David White is a community-based family doctor in Toronto and Associate Professor of Family & Community Medicine at the University of Toronto. (DFCM, U of T). He currently serves as the Interim Director of UTOPIAN, the practice-based research network comprising all teaching sites affiliated with the Department of Family & Community Medicine at the University of Toronto.
He obtained his medical degree and completed residency in Family Medicine at the University of Toronto. He began clinical practice in 1977 at Sioux Lookout, working at the Zone Hospital and flying into remote First Nations villages in northwestern Ontario. In this setting he began a long-term affiliation with U of T. On returning to Toronto in 1980, he joined the Family Medicine Teaching Unit at Toronto Western Hospital, and later moved to Mount Sinai Hospital. In 1999 he was appointed Chief of Family & Community Medicine at North York General Hospital (NYGH).
His current academic activities include clinical teaching in his community office and in obstetrics, research in health care delivery, and mentoring of junior faculty. Contact Dr. White
Tags
Breastfeeding Media Mental Health Maternal Mental Health Maternity Care Penny Simkin Epidurals And Postpartum Depression ChildBirth In The Media Maternal Safety Evidence Based Teaching Guest Posts Maternity Care Research Birth Advocate David White MD Post