April 10, 2011
Journal of Perinatal Education 20.1 Feature Article: Umbilical Cord Blood: Information for Childbirth Educators
By: Kimmelin Hull, PA, LCCE | 0 Comments
The Spring 2011 issue of the Journal of Perinatal Education (JPE 20.1) has already landed in your mailbox and is now available on-line.  As always, it is chock-full of illuminating and informing articles about perinatal health care issues. Considering our recent re-post of Dr. Nicholas Fogelson's Grand Rounds lecture on delayed umbilical cord (UC) cutting and clamping, the continuing education module contained in this issue of the JPE caught my attention:Umbilical Cord Blood: Information for Childbirth Educators by Renece Waller-Wise, MSN, CNS, CLC, CNL, LCCE.
As always, it is chock-full of illuminating and informing articles about perinatal health care issues. Considering our recent re-post of Dr. Nicholas Fogelson's Grand Rounds lecture on delayed umbilical cord (UC) cutting and clamping, the continuing education module contained in this issue of the JPE caught my attention:Umbilical Cord Blood: Information for Childbirth Educators by Renece Waller-Wise, MSN, CNS, CLC, CNL, LCCE.
As options for UC collection and banking/donation are increasing, questions about efficacy and indications grow. Waller-Wise does a tremendous job in her article providing not only the background on stem cell research (dating back to the 1950s) and transplant and collection (1980s and 1990s, respectively) but she reviews the illnesses that are currently amenable to treatment with umbilical cord blood stem cell transplantation along with the advantages and disadvantages of employing this treatment modality.
While the use of umbilical cord blood stem cells to treat previously identified familial illness in a first degree relative provides a primary indication for collection and banking, the procedure and storage is costly, the cells have a definitive shelf life and success of transplant is not necessarily guaranteed (see Waller-Wise's article for details). And the chance of using these stem cells for treatment at all? At best, the likelihood is estimated to be 1 /2,700.[1]
Beyond whether or not cord blood banking is a reasonable "insurance policy" to invest in, another debate is ensuing which heightens the gravity of the following questions: "Should we, or should we not retrieve UC blood at all? And if so, should the commonly accepted practices surrounding cord blood collection be altered?"
In Dr. Fogelson's Grand Rounds videos, his message is clear: immediate clamping and cutting of the umbilical cord deprives the newborn of nearly 20mL/kg of her potential blood volume. As Fogelson describes it, "...by clamping the umbilical cord [early] you phlebotomize the baby of 40% of its blood volume." Dr. Fogelson goes on to explain the various suspected and documented morbidities associated with newborns who have been deprived of this extra (read: nature-intended) blood volume.
Renowned family practice and obstetrics physician, Dr. Sarah Buckley, echoes these concerns in her seminal book, Gentle Birth, Gentle Mothering: A Doctor's Guide to Natural Childbirth and Gentle Early Parenting Choices. Dr. Buckley expands upon the risks of early umbilical cord cutting and clamping this way:
"Active management [of the Third Stage] also creates specific difficulties for mother and baby. In particular, active management can lead to the deprivation of one third,
on average, of a newborn's expected blood volume. When active
management is used, this extra blood, intended to perfuse the newly
functioning lungs and other vital organs, is discarded along with the placenta.
Possible consequences include breathing difficulties and anemia,
especially in vulnerable babies; long-term effects on brain development
are also very plausible."[2]
But how much of this placental blood is the newborn really deprived of during UC blood collection?
Depending on the system used (needle + syringe extraction vs. needle + dependent bag collection) along with provider skill/preference, cord blood collection requires between 40-200mL of blood such that an adequate volume of stem cells might be retrieved, processed, and made available for transplant. This volume, incidentally, is on par with the amount of blood a newborn can receive via placental transfusion when the cord is left patent for at least three minutes after birth. (See Dr. Buckley's and Dr. Fogelson's works, referenced above.) Because of this, common practice is to immediately clamp the umbilical cord following the baby's birth and initiate cord blood collection moments later - capturing every drop of blood possible into the collection device.
The question, then, becomes: does the benefit of potentially successful treatment of current familial illness, or future autologous UC blood stem cell transplantation, outweigh the risk of significant newborn phlebotomization?
Before jumping into this debate, my heart tells me there is a third option.
Google "cord blood withdrawal without clamping" and you will find message board and blog site discussions like this one where anecdotal evidence is beginning to emerge and become the subject of hot debate: it just might be possible to delay clamping & cutting the umbilical cord and collect a cord blood sample that satisfies requirements for banking/transplantation purposes. Make no mistake: I am not presenting these discussions as science, evidence or infallible support for creating a new Third Stage practice. I am simply relaying what some maternity care providers have begun doing on their own. (Isn't that how medical advances have developed in the past? Someone tries something new and, low and behold it works...leading to the adoption of the new practice by others?)
The catch, of course, if how much UC blood can be collected after delayed clamping, and whether collection can take place before clotting sets in within the cord/placenta. One maternity care provider respondent on the Mothering.com message board offered a depiction of howshe goes about collecting cord blood after placental delivery:
"The bag is about 500mL, I can usually get about 1/3 of a bag, so a bit more than 150mL, even after the placenta is born. I usually put the placenta on a counter top, with the bag resting on the floor, start low by the clamp and move up the cord, and use all those juicy veins on the fetal side of the placenta. If you elevate the placenta with the cord hanging, quite a bit will flow into the cord. Obviously, you're not going to get a full 500mL if you wait for the birth of the placenta, but you can get a decent amount with a little patience and multiple sticks. And you don't want to wait too long after the birth of the placenta, or the blood coagulates, so someone else should be watching mama and baby while the other does the collection."
If the practice described above is truly reproducible, it would suggest that there is plenty of cord blood available (and perhaps more than what has been previously assessed).
In 2007, the American Academy of Pediatrics released a statement providing the following guidance as a part of its endorsement of cord blood banking when known familial illnesses treatable by stem cell transplant exist:
"The cord blood stem cell-collection program should not alter routine practice for the timing of umbilical cord clamping."[3]
ACOG's Committee Opinion paper #399 (Feb '08), Umbilical Cord Blood Banking offers the same guidance. [1]
If we can all agree that in most cases, delaying the clamping and cutting of the umbilical cord constitutes the best, evidence-based practice, then the above AAP statement ought to apply to cord blood collection after a sufficient amount of time has transpired for placental transfusion to take place.
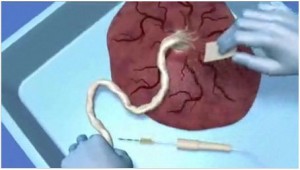
If you look on the website* of one of the largest cord blood banking companies, you can watch a demonstration of umbilical cord blood collection - complete with instructions on how to collect an adequate volume after the birth of the placenta:
The AAP along with ACOG now advise maternity care providers to counsel interested patients on the risks and benefits of cord blood banking. Factors such as the likelihood of actually using the stem cells, philanthropic drive to donate stem cells to public cord blood banks and the cost of collection and storage should all be taken into consideration when expectant parents are contemplating this choice. As should the importance of what that added blood volume can do for the newborn whose body is undoubtedly expecting it. And I, for one, can't help but to believe a viable third option exists in which the newborn is granted the lion's share of the placental transfusion while a small and remaining amount is collected for cord blood banking, when the proper indications are present.
Surely a study can be formed to test this hypothesis.
To learn more about umbilical cord blood collection and storage, go here to read Waller-Wise's full article (compliments of the Journal of Perinatal Education and Springer Publishing) and don't forget to take the post test to earn continuing education credits!
[1]Umbilical cord blood banking. ACOG Committee Opinion No. 399. American College of Obstetrics and Gynecologists. Obstet Gynecol 2008;111:475-7
[2] Gentle Birth, Gentle Mothering : A Doctor's Guide to Natural Childbirth and Gentle Early Parenting Choices by Sarah J Buckley MD (Celestial Arts, Berkeley CA,2009) p 156;www.sarahbuckley.com
[3] http://aappolicy.aappublications.org/cgi/content/full/pediatrics;119/1/165; Recommendations #7
*Neither Lamaze International nor the editor or contributing writers to Science & Sensibility endorse any particular cord blood bank or registry organization or company.
Posted by: Kimmelin Hull, PA, LCCE
Tags
Cord Blood Banking Babies American Academy Of Pediatrics Position On Cord Bl Benefits And Risks Of Cord Blood Banking Cord Blood Registry Cord Blood Stem Cell Collection Delayed Cord Clamping And Cutting How To Collect Umbilical Cord Blood