January 04, 2016
Dueling Statistics: Is Out-of-Hospital Birth Safe?
By: Henci Goer, BA | 0 Comments
By Henci Goer
'[T]he best evidence in answer to the wrong question is useless.' Menticoglou & Hall 2002
Last week, a new study was published in the New England Journal of Medicine titled 'Planned out-of-hospital birth and birth outcomes.' This study looked at the safety of home birth using Oregon State birth certificate data and once again brought up the unclear debate on the safety of home birth. Many experts agreed that the study was well done, but why is this research not returning the same results as other well conducted previous home birth studies? Henci Goer, author and recognized expert on the topic of childbirth does an excellent job in comparing and contrasting this newest study with other recent home birth analyses, including the 2015 Canadian study that demonstrated different results. Henci helps S&S readers to understand why this might be. On Thursday, Jeanette McCulloch of BirthSwell interviews Melissa Cheyney, PhD, CPM, LDM and the Chair of the Midwives Alliance Division of Research, on her perspective on how childbirth educators can help families interpret the new study when making their own decisions about place of birth. ' Sharon Muza, Science & Sensibility Community Manager
 Within weeks of each other, two studies of out-of-hospital (OOH) birth were published that came to opposite conclusions on the safety of OOH birth for babies. On the one hand, we have Hutton et al. (2015), a Canadian study. Hutton compared 11,493 planned home births at labor onset attended by midwives matched to women who would have been eligible for home birth but planned hospital births with those same midwives. (Ontario, unlike the U.S., has an integrated system in which midwives move freely between home and hospital.) On the other hand, we have Snowden et al. (2015), an analysis of Oregon State birth certificate statistics collected after the question, 'Did you go into labor planning to deliver at home or at a freestanding birth center?' was added to the birth certificate. This question enabled investigators to distinguish hospital transfers and assign outcomes to the correct category as well as exclude unplanned home births. (Unplanned home births shouldn't be included if one is trying to determine the safety of planned OOH birth.) Snowden compared 3203 births planned at freestanding birth centers or at home at labor onset with 79,727 planned hospital births. All women were at term (> 37 weeks) with a single, head-down baby free of congenital anomalies.
Within weeks of each other, two studies of out-of-hospital (OOH) birth were published that came to opposite conclusions on the safety of OOH birth for babies. On the one hand, we have Hutton et al. (2015), a Canadian study. Hutton compared 11,493 planned home births at labor onset attended by midwives matched to women who would have been eligible for home birth but planned hospital births with those same midwives. (Ontario, unlike the U.S., has an integrated system in which midwives move freely between home and hospital.) On the other hand, we have Snowden et al. (2015), an analysis of Oregon State birth certificate statistics collected after the question, 'Did you go into labor planning to deliver at home or at a freestanding birth center?' was added to the birth certificate. This question enabled investigators to distinguish hospital transfers and assign outcomes to the correct category as well as exclude unplanned home births. (Unplanned home births shouldn't be included if one is trying to determine the safety of planned OOH birth.) Snowden compared 3203 births planned at freestanding birth centers or at home at labor onset with 79,727 planned hospital births. All women were at term (> 37 weeks) with a single, head-down baby free of congenital anomalies.
What were their findings? Snowden found an excess of 0.9 more fetal (antepartum + intrapartum), 1.2 more perinatal (fetal + neonatal), and 0.8 more neonatal (death occurring by 28 days) deaths per 1000 in the population planning OOH birth after statistical adjustments for factors such as prior birth, prior cesarean, maternal health status (hypertension, diabetes), and demographic factors such as age, race, education, and payment source. In contrast, Hutton found no differences in intrapartum deaths, perinatal deaths (intrapartum + neonatal death), or neonatal deaths.
Both studies reported fewer cesarean surgeries in the OOH population. Snowden reported 24 fewer per 100 women, and Hutton reported a much smaller excess (2 per 100 in both first-time mothers and women with prior births, some of whom had prior cesareans), but this would be expected since women planning home births and women planning hospital births were attended by the same midwives whereas women planning hospital births in the Snowden study would mostly have been attended by obstetricians. The interesting thing is that Hutton found a difference at all, but that's a discussion for another day.
These two studies join a parade of studies of OOH birth that reach contradictory conclusions on perinatal outcomes and agree that OOH birth reduces cesarean surgeries, a severe adverse outcome in its own right on the maternal side with potential for severe adverse perinatal outcomes down the line (Goer 2012a). I contend that it's time to stop asking 'Is it or isn't it?' questions of OOH birth because it's pretty clear that the answer is 'It depends.' I think a much more useful question is . . .
'What Factors Influence Outcomes?'
To attempt an answer, I would like to compare and contrast Hutton and Snowden along with a couple of other studies that, like them, are well-conducted studies of OOH birth in a physician-led system of maternity care. One of them uses Midwives Alliance of North America (MANA) data to analyze outcomes in 16,924 U.S. women planning home births at labor onset (Cheyney 2014). The other uses American Association of Birth Centers (AABC) data to analyze outcomes in 15,574 women planning birth at freestanding birth centers at labor onset (Stapleton 2013).

As you can see, mortality rates are higher in the Snowden study compared with the same statistic in the other three. One possible explanation may lie in the limitations of harvesting data from birth certificates. The other three studies collected data from forms designed for evaluating OOH birth. Snowden et al. point out the potential for inaccuracy, citing as an example that 27 women among the 601 transfers reported that they had planned OOH births with physicians, which is undoubtedly a recording error. One wishes, too, for more detailed information on causes and timing of death. Stapleton reports 14 fetal deaths of which five were diagnosed on arrival at the birth center and the women immediately transferred to the hospital and another two that were born at the birth center because the women arrived too close to delivery to transfer. Snowden reports ten fetal deaths, two delivered at home and eight in the hospital. Could some of Snowden's cases likewise be an antepartum demise? We don't know. Nor do we know whether any of the five neonatal deaths Snowden reports were unrelated to planned birth setting.
Let's assume, though, that the varying mortality rates among studies is at least partially attributable to factors other than the limitations of the data source. What else might these be? Snowden and colleagues' thoughtful, fair minded discussion of their results helps us out here too.
They observe that the home birth attendant's qualifications may be one. Three percent of their OOH births were home births attended by people with no qualifications such as relatives, and another 13% were attended by midwives who were neither Certified Nurse Midwives (CNMs) nor Certified Professional Midwives (CPMs). Cheyney, which, as you can see, reported intrapartum mortality rates greater than Hutton's, found that 6% of their population were attended by non-credentialed midwives. All women in Hutton were attended by registered midwives (RMs). Snowden and colleagues point out that a movement is underway in the U.S. to bring all U.S. midwifery training in line with the standards of the International Confederation of Midwives (ICM). I can add that the movement is accompanied by efforts to legalize CPM-credentialed midwives in all states. Giving women access to licensed, regulated, credentialed midwives in every state should reduce the use of less qualified OOH birth attendants.
Snowden also notes that integrating OOH midwifery into the maternity care system could make a difference. Cheyney and colleagues agree. They write: 'The lack of integration across birth settings . . . contributes to intrapartum mortality due to delays in timely transfer related to fear of reprisal' (p. 9). Supportive of this is that while Cheyney's intrapartum mortality rates exceed Hutton's, neonatal mortality rates are identical and similar to the neonatal mortality rates Hutton reports in its hospital population. It could be argued that Stapleton is a U.S. study too, and despite a non-integrated system, it has very low mortality rates, to which I would respond that birth centers are more likely to have formal relationships with physicians and hospitals than home birth midwives.
What, I wonder, might we find if researchers attempted to answer my proposed research question? What if they pooled data from these four studies and compared perinatal mortality and other serious adverse outcomes according to:
- Credentialed or licensed vs. non-credentialed care provider
- Credentialed or licensed care provider in an integrated vs. non-integrated system, including Stapleton in the integrated arm.
Admittedly, even the combined data probably wouldn't have sufficient numbers to detect statistically significant differences between groups, and even if it did, association doesn't mean causality. Still, Hutton's and Stapleton's findings suggest that OOH birth with qualified home birth care providers practicing in an integrated system results in perinatal loss rates no greater than in similar women planning hospital birth.
There's still more. Snowden and colleagues note as well that banning hospital VBAC pushes women wanting to avoid elective repeat surgery into OOH birth, potentially to their detriment (and kudos to them for not blaming the victims). It wouldn't be worthwhile to explore what factors might affect perinatal outcomes in OOH VBAC because only Cheyney has a sizeable number of them. That being said, some of the perinatal deaths in Cheyney's population were in women having home births after cesareans (HBACs) (Cox 2015).
So what's the bottom line here? The only factor the OOH community controls is the qualifications of its providers, and as I wrote above, work is proceeding on bringing those in line with ICM standards.
The other factors, providing a system in which OOH care providers can readily consult, collaborate, and transfer care and where VBAC is not only available on demand but managed in ways that best promote safety and maximize vaginal births, depend on the obstetric and hospital community. The OOH community is doing its part. It's time for the obstetric community to step up to the plate and do theirs. But we're not done until we also ask . . .
'What about the Risks of Planned Hospital Birth?'
This brings us to the other side of ledger. Cheney and colleagues observe that another reason that women with risk factors choose OOH birth is that they can't find in-hospital care that supports physiologic birth. We have abundant evidence of the gross overuse of tests, drugs, restrictions, and procedures in hospitals, the toll of its consequent harms, and the low use of practices known to promote healthy, physiologic birth (Declercq 2006; Declercq 2013; Goer 2012). As we saw above, 24 fewer women per 100 in Snowden planning OOH birth had cesareans compared with women planning hospital birth, most of whom would have had obstetricians as care providers, while only two more women per 100 had cesareans in Hutton, where women planning hospital birth had midwife-led care. And as this chart from Listening to Mothers III, a national U.S. survey, makes clear, excess cesarean surgeries don't occur in a vacuum.
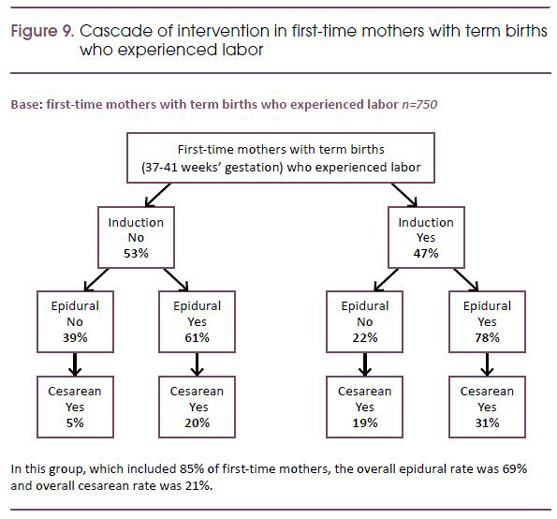
© Listening to Mothers III, Declercq 2013
Indeed, a good case could be made that the answer to the question 'Is hospital birth safe for the low-risk woman?' is 'No.' In light of that fact, the obstetric community should stop paying so much attention to the speck in their neighbor's eye and attend to the beam in their own. If they did, everyone would benefit. Fewer women would feel the need to opt out of the hospital, and the 99% of women who plan hospital birth would be infinitely better off. It's a win-win.
Bibliography
Cheyney, M., Bovbjerg, M., Everson, C., Gordon, W., Hannibal, D., & Vedam, S. (2014). Outcomes of care for 16,924 planned home births in the United States: the Midwives Alliance of North America statistics project, 2004 to 2009. J Midwifery Womens Health, 59(1), 17-27.
Cox, K. J., Bovbjerg, M. L., Cheyney, M., & Leeman, L. M. (2015). Planned Home VBAC in the United States, 2004-2009: Outcomes, Maternity Care Practices, and Implications for Shared Decision Making. Birth.
Declercq, E., Sakala, C., Corry, M. P., & Applebaum, S. (2006). Listening to Mothers II: Report of the Second National U.S. Survey of Women's Childbearing Experiences. New York: Childbirth Connection.
Declercq, E., Sakala, C., Corry, M. P., Applebaum, S., & Herrlich, A. (2013). Listening to Mothers III. Pregnancy and Birth. New York: Childbirth Connection.
Goer, H., & Romano, A. (2012). Optimal Care in Childbirth: The Case for a Physiologic Approach. Seattle, WA: Classic Day Publishing.
Goer, H., Romano, A., & Sakala, C. (2012a). Vaginal or cesarean birth: What is at stake for women and babies? A best evidence review. Retrieved from New York: http://transform.childbirthconnection.org/reports/cesarean/
Hutton, E. K., Cappelletti, A., Reitsma, A. H., Simioni, J., Horne, J., McGregor, C., & Ahmed, R. J. (2015). Outcomes associated with planned place of birth among women with low-risk pregnancies.CMAJ.
Menticoglou, S. M., & Hall, P. F. (2002). Routine induction of labour at 41 weeks gestation: nonsensus consensus. BJOG, 109(5), 485-491.
Snowden, J. M., Tilden, E. L., Snyder, J., Quigley, B., Caughey, A. B., & Cheng, Y. W. (2015). Planned out-of-hospital birth and birth outcomes. New England Journal of Medicine, 373(27), 2642-2653.
Stapleton, S. R., Osborne, C., & Illuzzi, J. (2013). Outcomes of care in birth centers: demonstration of a durable model. J Midwifery Womens Health, 58(1), 3-14.
About Henci Goer
Henci Goer, award-winning medical writer and internationally known speaker, is the author of The Thinking Woman's Guide to a Better Birth and Optimal Care in Childbirth: The Case for a Physiologic Approach, She is the winner of the American College of Nurse-Midwives 'Best Book of the Year' award. An independent scholar, she is an acknowledged expert on evidence-based maternity care. Henci is preparing to launch Childbirth U in the first quarter of 2016.
Tags
Research VBAC Home Birth Professional Resources Labor/Birth Newborns Henci Goer MANA Home Birth Safety Hutton Neonatal Mortality Snowden